What is a hysterectomy?
If you’re facing the possibility of a hysterectomy, it’s completely normal to have a lot of questions and emotions swirling around. Together, we’ll explore what a hysterectomy is, the different types, and common reasons why someone might need one.
We’ll also take a look at common concerns like how the surgery might affect your hormones, your fertility and even how it might impact your emotional wellbeing. Every question is important, and you deserve to feel informed, supported, and understood as you navigate this journey.
So, what’s a hysterectomy?
A hysterectomy is a surgery to remove the uterus, though it may also involve removing other parts of the reproductive system, such as the cervix (the part of the uterus that connects to the vagina), ovaries (two small glands that produce eggs and hormones), or fallopian tubes (a pair of tubes that carry eggs from the ovaries to the uterus). This type of procedure is recommended to treat certain health conditions, but the specifics can vary based on your individual needs.
What types of hysterectomy surgery are there?
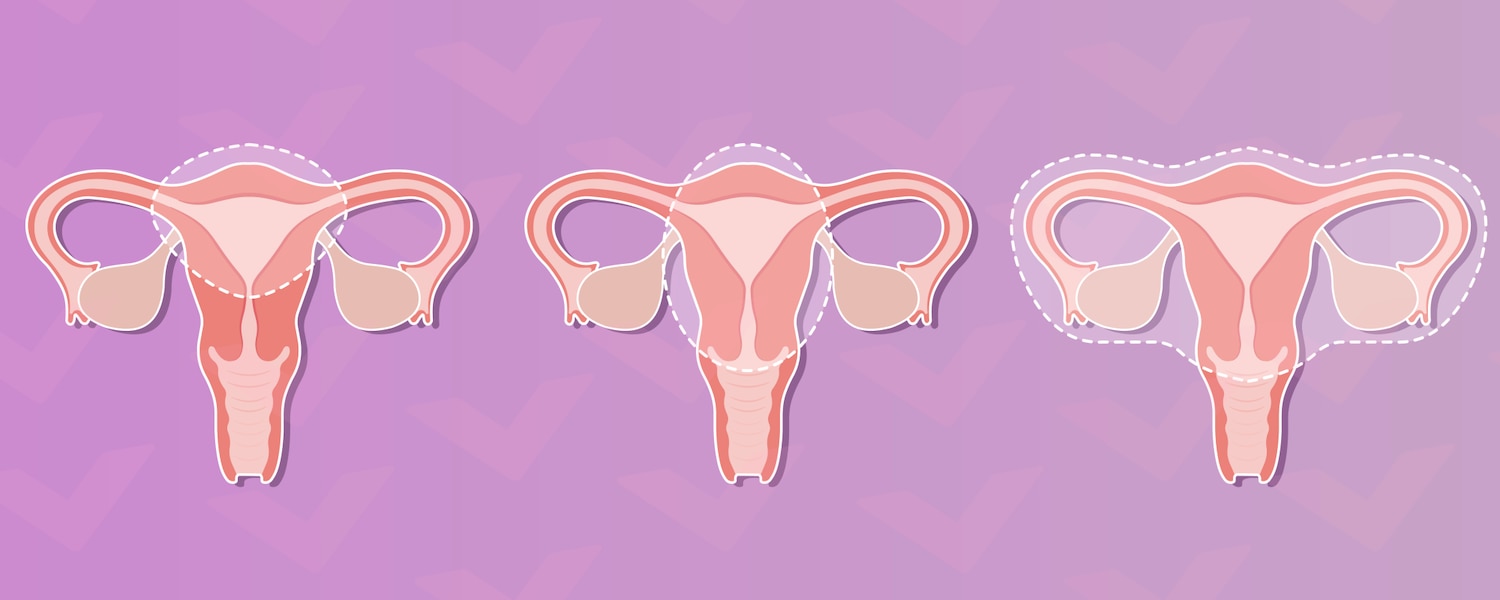
The three types are different based on what is removed in a hysterectomy:
- Partial hysterectomy: Also known as a subtotal hysterectomy, this involves removing the uterus while leaving the cervix intact. It's often chosen for conditions affecting only the uterus, such as uterine fibroids or uterine prolapse.
- Total hysterectomy: The most common type of hysterectomy, this procedure involves removing the entire uterus and cervix, but not the ovaries.[1] This is a common treatment option for a variety of health issues, including severe endometriosis, chronic pelvic inflammatory disease (PID), and certain types of cancer. You might sometimes hear it called a complete hysterectomy or simple hysterectomy.
- Radical hysterectomy: This type involves the removal of the uterus, cervix, part of the vagina, lymph glands and surrounding tissues. It's usually performed in cases of cancer.
Understanding these options can help you have a clearer conversation with your doctor about what might be best for your specific situation. Remember, each person’s journey is unique and what's right for someone else might not necessarily be what's right for you.
Why would someone need a hysterectomy?
There are several reasons why someone might need a hysterectomy, most commonly as a treatment for certain medical conditions. Hysterectomies are a big deal, so you'll usually try other treatments first to see if they solve your issues.
Hysterectomies are used as a treatment option for a wide range of conditions, including: [2]
- Fibroids: Non-cancerous growths in the uterus that can cause pain and heavy bleeding.
- Adenomyosis: A condition that can cause the uterus to grow larger than usual, which can lead to heavy periods.
- Endometriosis: A condition where tissue similar to the lining of the uterus grows outside of it, leading to discomfort and complications.
- Chronic pelvic pain: Ongoing pain in the pelvic area that hasn’t responded to other treatments.
- Abnormal bleeding: Heavy or irregular bleeding that can disrupt daily life that hasn't responded to other treatments.
- Cancer or precancerous conditions: Diagnosis of cancer or if abnormal cells are found in the reproductive organs (ovarian cancer or cervical cancer, for example).
Ultimately, the goal is to improve your health and quality of life, but making any big decision about your health and fertility can be scary. But, your healthcare provider is there to talk you through everything and help you decide if a hysterectomy is the right option for you.
How is a hysterectomy performed?
Understanding how a hysterectomy is performed can help ease any worries you might have about the procedure. Typically, there are a few methods your surgeon might use, depending on your individual situation:
- Abdominal hysterectomy: This type of surgery is done through a cut along the lower part of your tummy, usually horizontal just along the bikini line, allowing the surgeon to access the uterus directly. It’s often chosen for more complex cases where a clear view is essential.
- Vaginal hysterectomy: In this approach, the uterus is removed through the vagina, which generally results in less scarring and a quicker recovery. This is usually performed for cases where the uterus can fit through the vagina.
- Laparoscopic hysterectomy: Also known as keyhole surgery, this minimally invasive procedure uses small incisions and a camera to guide the surgeon as they remove the uterus. Laparoscopic surgery often leads to shorter recovery times and less post-surgery pain.
During the surgery, you’ll be put to sleep, so you won’t feel anything. Then, after the procedure, your healthcare team will monitor you as you begin the recovery process. Recovery times vary depending on the type of procedure, and everyone heals at their own pace, so it’s completely normal to recover a bit slower or faster than others. Knowing what to expect can make a big difference, and connecting with others who’ve been through it can be really reassuring. Online forums and communities are full of people who can support you, from sharing their experiences from start to finish or just to tell you it will all be okay.
Is having a hysterectomy safe?
A hysterectomy is generally considered a safe procedure, and many people in their 40s and 50s undergo it to improve their health and quality of life.[3] Like any surgery, it does come with risks, but they are quite rare.
You can always talk to your doctor, gynaecologist or surgeon so they can explain these risks and help resolve any concerns you might have. The idea of having surgery can be scary, but just remember that the improvement it can make to your life will be worth it if you choose to take this step.
Can I have a hysterectomy by choice?
Yes, you can choose to have a hysterectomy, and it’s perfectly okay to consider this option for personal reasons. Some people might want a hysterectomy to manage chronic pain, heavy bleeding, or other health issues that significantly impact their everyday lives. Others might choose it as a way to reduce the risk of certain conditions, like cancer, especially if these conditions run in their family. Hysterectomies and other surgical procedures, like tubal ligation, can also be used as a permanent form of birth control.
If you’re thinking about a hysterectomy for personal reasons, it’s important to have an open conversation with your gynaecologist. They can help you weigh the benefits and risks and discuss any other options that might be available such as medications or other procedures like endometrial ablation (removing the lining of your uterus). Remember, a hysterectomy is a major surgery. So take some time, talk to friends and family about how you're feeling and feel confident in your choice. Ultimately, the decision is yours, just make sure you've considered all of your options before making the best choice for you.
Does a hysterectomy stop periods?
Since the surgery involves removing the uterus (a key player in your menstrual cycle), you won’t have periods anymore. This can be a significant relief for many people who experience heavy or painful periods.
If you have a total hysterectomy, which also removes the cervix, you’ll definitely notice the end of your periods. However, if you’re having a partial or subtotal hysterectomy where the cervix isn't removed, you won’t have periods, but you might still have some spotting, similar to a light period.[4]
If you experience heavy bleeding after a hysterectomy and are concerned about it, it might be a good idea to see your gynaecologist. They can check everything is okay and give you peace of mind.
Can I have children after a hysterectomy?
If you have a hysterectomy, it means you won’t be able to carry a pregnancy, as the uterus is where a baby develops during pregnancy. This can be a difficult realisation for you, especially if starting or growing a family is part of your hopes and dreams. It’s completely natural to feel a mix of emotions about this and even feel a sense of loss and grief.
If you're struggling with the emotional effects of this change, reaching out to friends, family, or even a counsellor can help you navigate this challenging experience.
The good news is that there are still other options for building a family if that’s something you want. You can consider alternatives like adoption, egg freezing or using a surrogate. This might not be the way you pictured having a family, but it can be just as fulfilling as having biological children. If this is something on your mind, talking with your healthcare provider can help you explore what options might be available and provide support as you navigate your feelings.
How will my hormones change after a hysterectomy?
If one or both of the ovaries are removed during the surgery (known as an oophorectomy) or the blood supply to them is affected, it can lead to a decrease in the production of hormones. This may cause what is known as surgical menopause. The symptoms of surgical menopause are similar to natural menopause, including hot flushes and night sweats, mood swings, or changes in sex drive.
However, if your ovaries are left intact, you might not experience significant hormonal changes since they continue to produce oestrogen and progesterone (your reproductive hormones). Everyone's experience is unique, and it's natural to have questions about how this might affect your body.
If you're worried about hormonal changes or menopause symptoms after a hysterectomy, it can really help to talk with friends or family — some might even be going through the same thing. If you want to find out more about possible treatment options like Hormone Replacement Therapy (HRT), have a chat with your doctor to see how they can help you.
Will I need to have smear tests after a hysterectomy?
Needing a smear test after a hysterectomy procedure depends on the type of procedure you have, particularly if your cervix is removed or not. Since smear tests are used to detect cervical cancer, if you no longer have a cervix, you won’t need to have them. However, if you still have your cervix, it might still be recommended for you to have a smear test. If you’re unsure about this, make sure you check with your doctor, as smear tests are an important part of your intimate health.
Hysterectomy surgeries are significant procedures, but for many, they can lead to better health and an improved quality of life, ranging from chronic pelvic pain relief to potentially life-saving cancer treatment. Having a clear understanding of how it works and what to expect is essential—whether it's preparing for the physical recovery or navigating the emotional challenges that can come with it. Being in the know about what to expect helps you feel more confident and supported as you manage both the physical and mental aspects of the experience. Recovering from a hysterectomy can be daunting at first and can result in complex feelings about your fertility. To find out more, check out what you can expect at different stages of your healing journey or learn why there's no shame in living child-free by choice.
Medical disclaimer
The medical information in this article is provided as an information resource only and is not to be used or relied on for any diagnostic or treatment purposes. Please consult your doctor for guidance about a specific medical condition.
This article has been reviewed on 6th January 2025 by Karen Joash BSc (Hons), MSc, MBBS, MRCOG PGCert, ILM and MBA, Consultant Obstetrician and Gynaecologist at Queen Charlotte's and Chelsea Hospital. You can find out more about Dr Karen on her Instagram, LinkedIn and X pages.
References:
[1] https://stanfordhealthcare.org/medical-treatments/h/hysterectomy/types.html
[2] https://www.kernodle.com/obgyn_blog/reasons-for-a-hysterectomy/
[3] https://mft.nhs.uk/app/uploads/sites/4/2018/04/99-13-Hysterectomy-Oct-2012.pdf
[4] https://www.esht.nhs.uk/wp-content/uploads/2018/07/0064.pdf


